If you have questions about the COVID-19 vaccine, we have compiled answers to the most frequently asked questions heard from patients. If you still have reservations about the safety and efficacy of these vaccines, we strongly urge you to rely on factual, science-based resources like ours. We are confident that once you get the facts, you’ll get the vax.
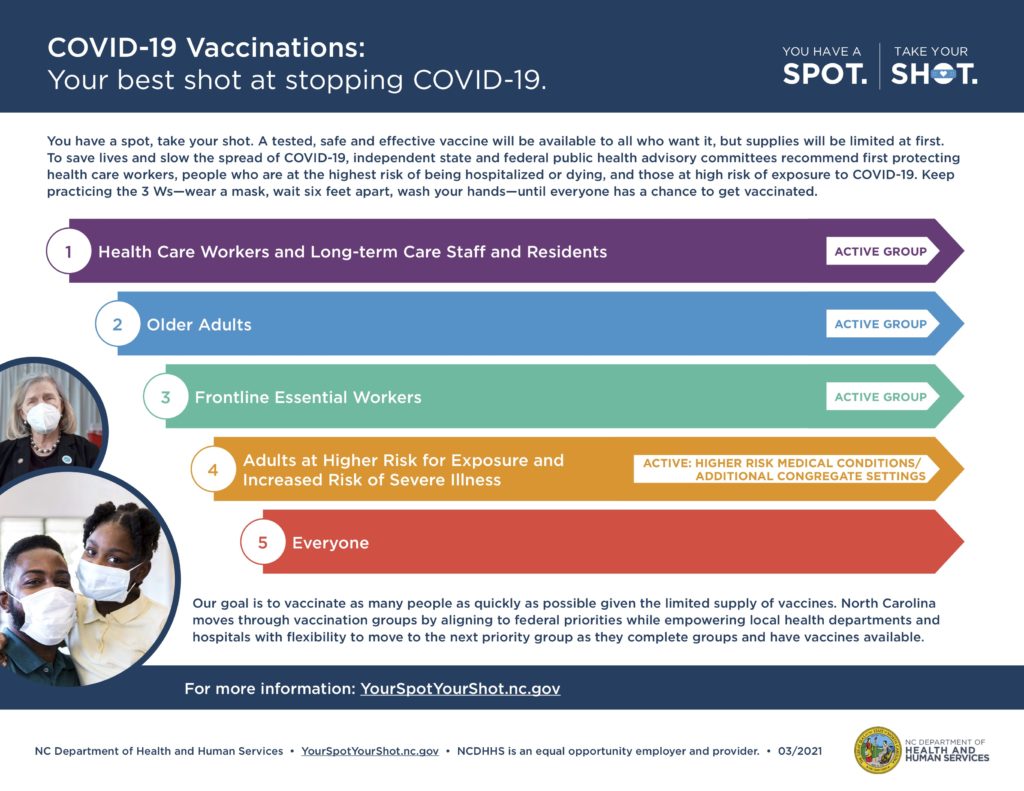
To learn more about vaccine distribution including where you can make an appointment and what group you’re in, click here.
Why People Should Be Vaccinated
It seems that vaccine production was rushed, how can that be safe?
The fact is that scientists had already been working on vaccine strategies for viruses just like coronavirus for several years prior to the appearance of COVID-19. In addition, the companies that produced the mRNA COVID vaccines have been studying mRNA technology for over a decade. However, the speed occurred because a global pandemic struck and governments rapidly funded vaccine trials and then put large amounts of money into manufacturing vaccines at a rapid rate. NO steps were skipped in the vaccine trials.
Does the vaccine change my DNA?
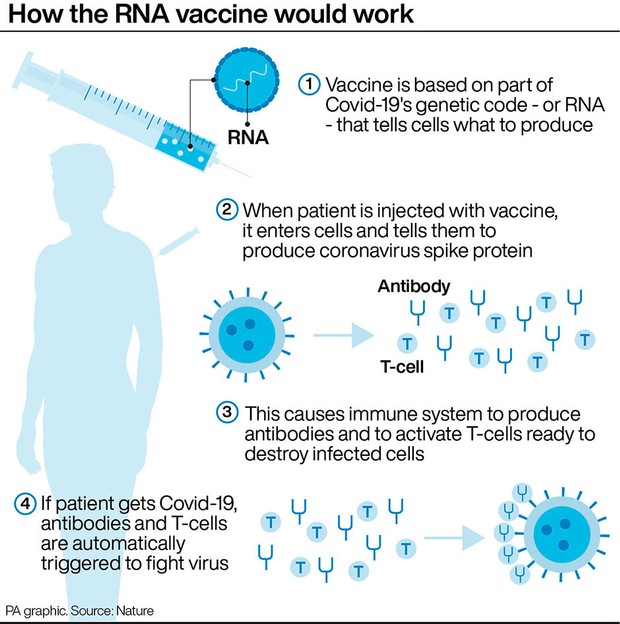
Absolutely not. All vaccines introduce a little piece of the virus into your body, which is not enough to make you sick. Your immune system then makes antibodies against that little piece so that when the real virus enters your body, the antibodies are ready to fight off the virus.
The mRNA vaccines provide the genetic “code” for surface pieces of the coronavirus. Once your cells have the genetic code, your body produces pieces of the virus protein and your immune system then makes coronavirus antibodies. The mRNA NEVER enters the cell nucleus where all your DNA is stored.
I’d rather wait to see how others do first…
Hundreds of thousands of people were immunized through all the vaccine trials across the world. If there had been any serious side effects or safety concerns, the vaccines would not have been approved.
Was the vaccine tested on people of diverse ethnic backgrounds? Was everyone in the vaccine trials healthy? How do I know it’s safe for me?
The Moderna and Pfizer vaccine trial participants included 20-25% Hispanic, 10% Black and 5% Asian volunteers. Both vaccine trials had 20-25% of participants over age 65, and 30-35% of patients were obese. 5-10% of participants had diabetes, COPD or heart disease.
Is there a concern about getting the vaccine while pregnant or could it impact my fertility?
Talk to your OB/GYN about getting the vaccine if you are pregnant. While numbers of pregnant individuals in the trials were small, there were no adverse events with the vaccine. The World Health Organization’s (WHO) recently recommended withholding COVID-19 vaccines from pregnant individuals unless they are at high risk of exposure, however we still believe the benefits outweigh any risk. There is no evidence that COVID-19 vaccines affect fertility.
Will we get to stop wearing masks after vaccination?
The vaccines are 94-95% effective after getting both doses, which is great news. However, we will need to keep wearing masks until enough people get vaccinated to protect the bigger population.
Questions About Receiving the Vaccine
Does my doctor think I should get the vaccine?
Yes, in general, we strongly recommend getting the COVID-19 vaccine when and where possible. If you are undergoing chemotherapy now, check with your oncologist for guidance.
If I was diagnosed with COVID-19, should I still get the vaccine? If so, when?
If you have had COVID-19, you can get the vaccine at least 30 days after diagnosis. You could possibly wait up to 90 days after the COVID-19 illness before getting the vaccine, but waiting 30 days is the minimum.
Can I contract COVID-19 after getting my first dose of the vaccine?
Yes, you can contract the COVID-19 illness, but not from the vaccine itself. This is why it is incredibly important to continue to wash your hands, wear your face mask and practice social distancing. You only obtain partial immune protection after the first COVID-19 vaccine and thus are still able to contract the COVID-19 illness.
If I contract COVID-19 after receiving my first vaccine shot should I delay getting the second shot?
If you contract COVID-19 after your first dose of the COVID-19 vaccine, you can receive your second dose as scheduled, or as soon as your quarantine is complete.
I am allergic to many medications, should I get the vaccine?
Even if you have a history of anaphylaxis, it is OK to get the COVID-19 vaccine. You will be monitored for 30 minutes after receiving your COVID-19 vaccine. If you have a history of anaphylaxis to a vaccine, please consult your physician before getting the COVID-19 vaccine.
Can I get the COVID-19 vaccine and my shingles vaccine near the same time?
Getting the shingles vaccine shortly before or after getting either dose of the COVID-19 vaccine will not impact the effectiveness of either vaccine. We do recommend spacing the vaccines out by at least 14 days because they both cause similar side effects and may be hard on your body. Prioritize your COVID-19 vaccine first!
Can l get the COVID-19 vaccine if l am currently taking a blood thinner medication (including Plavix and Warfarin)?
Yes, you can. When you go to get your vaccine, let the person giving you the shot know so they can apply extra pressure to prevent bleeding after your vaccination.
If I am undergoing cancer treatment, or am on immunosuppressant drugs, is it safe for me to get the COVID-19 vaccine?
If you are undergoing cancer treatment, be sure to speak with your oncologist. If you are not in active treatment, you should proceed with getting the COVID-19 vaccine. If you are on immunosuppressants, speak with your doctor about vaccination and timing.
References:
- FDA Briefing Documents, Moderna Covid 19 Vaccine, 12/17/20
- FDA Briefing Documents, Pfizer-BioNTech Covid 19 Vaccine, 12/10/20
- “The Race to Save the World,” Walter Iaacson, Time Magazine, 1//18/21
- mRNA Vaccine: Facts vs Fiction, Toks Falarin, MD
- Graphic from Nature magazine
- ACOG and SMFM Joint Statement on WHO Recommendations Regarding COVID-19 Vaccines and Pregnant Individuals